The Truth About Spinal Cord Stimulation: Is It Right for Buckhead Patients?
Chronic pain has a way of shrinking your world. It’s not just the discomfort in your back, legs, or joints—it’s the way pain changes your sleep, your mood, your patience, and your relationships. It can turn simple routines into exhausting decisions: Can I sit through dinner? Will I pay for it tomorrow? Over time, pain stops being an occasional problem and starts feeling like a constant companion.
In Buckhead, many patients look for advanced solutions because they want more than a cycle of short-term fixes or constant medication. They want steady, dependable relief—and they want it in a way that supports daily life, not one that creates new concerns about side effects or long-term dependence.
It’s also completely normal to hesitate when you hear the words spinal cord stimulation. A common reaction is: “Is a device really the next step?” That’s a fair question—and it deserves a clear, honest answer. Spinal cord stimulation (SCS) isn’t for everyone, but for the right patient, it can be a meaningful, life-changing option.
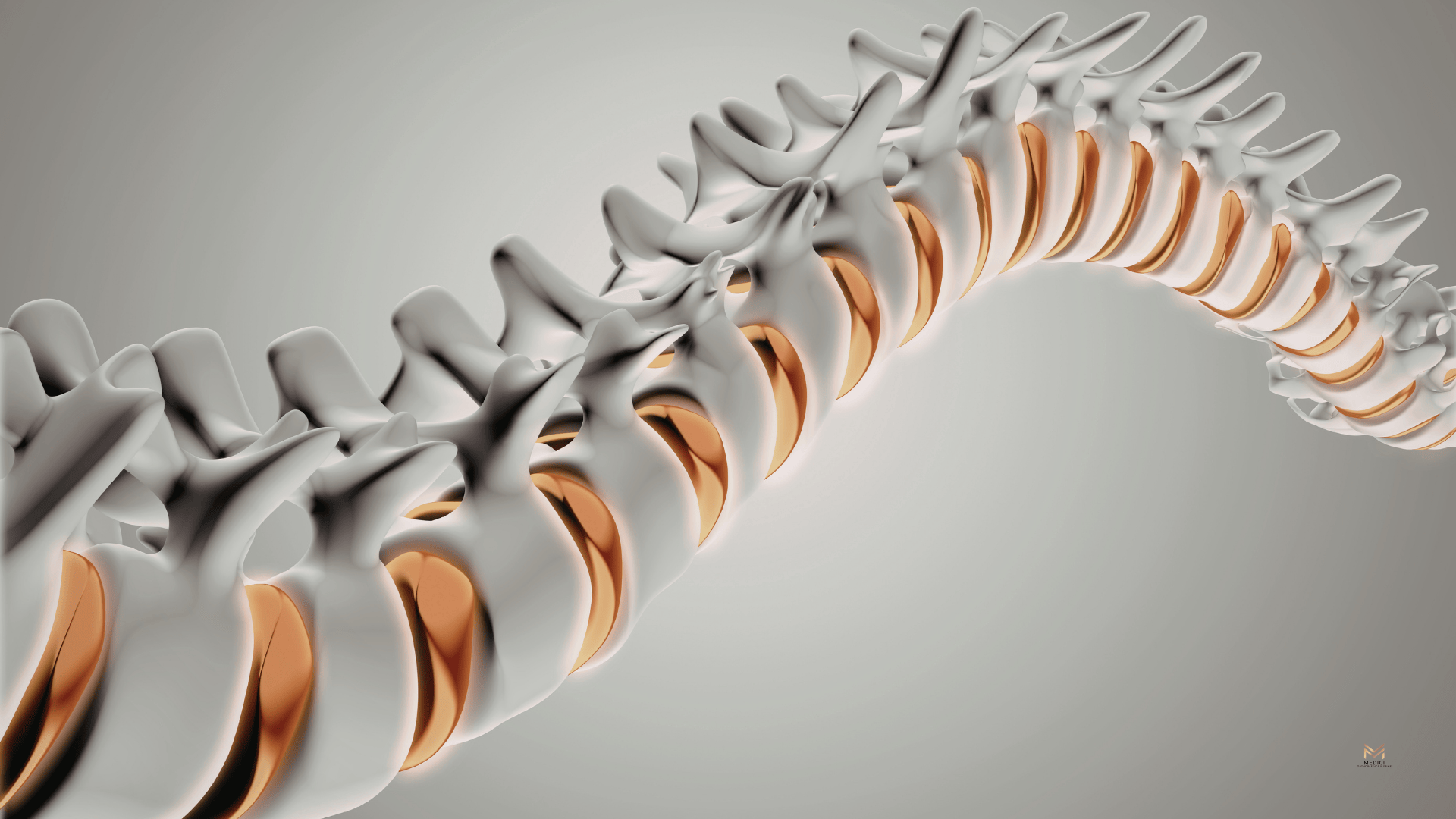
What Is Spinal Cord Stimulation?
Spinal cord stimulation is a treatment designed to help manage chronic pain—especially nerve-related pain—by changing how pain signals are processed. Instead of “fixing” a disc or joint directly, SCS focuses on the nervous system, where many chronic pain signals originate and persist.
When nerves are irritated or damaged, they can send persistent pain signals to the brain—signals that may feel like burning, shooting, electrical pain, or intense sensitivity. Spinal cord stimulation works by delivering mild electrical impulses near the spinal cord. These impulses help interrupt or modify pain signals before they reach the brain, which can reduce how intensely you feel the pain.
What the SCS System Includes
While different systems vary, spinal cord stimulation generally includes:
- A small implanted device (generator)
This is the power source, placed under the skin (often in the upper buttock or abdomen area, depending on the plan and body type). - Thin wires/leads placed near spinal nerves
These leads deliver the electrical stimulation to the targeted area near the spine. - A programmer/remote for patient control (as appropriate)
Many systems allow patients to adjust settings within safe parameters, helping tailor comfort to daily activities like walking, sitting, or sleeping.
Which Types of Pain Can Spinal Cord Stimulation Help?
Pain Patterns That May Respond Well
SCS may be considered for people experiencing:
- Nerve pain
Burning, shooting, electric sensations, or hypersensitivity that doesn’t respond well to standard treatments. - Radiating back/leg pain (sciatica-like symptoms)
Especially when nerve-related leg pain remains persistent despite conservative care. - Post-surgical pain
Including post-laminectomy syndrome / failed back surgery syndrome, where pain continues even after spinal surgery. - Complex Regional Pain Syndrome (CRPS)
A severe pain condition often marked by hypersensitivity, swelling, or changes in skin temperature/color. - Certain neuropathies (case-dependent)
Including diabetic neuropathy in select situations, particularly when symptoms are significant and resistant to other treatments.
Why SCS Is Usually Better for Nerve Pain Than Mechanical Pain
Mechanical pain typically comes from structural issues—like joint degeneration, instability, or muscle strain—and often behaves like aching, stiffness, or pain with specific movements. Neuropathic pain, on the other hand, is driven by nerve signaling and sensitivity.
Because SCS targets pain signaling, it tends to help more when nerve pathways are the primary driver. If pain is mostly mechanical, other approaches may be more effective (such as targeted rehabilitation, interventional treatments, or regenerative options where appropriate).
Signs You Might Be a Candidate for SCS in Buckhead
Your Pain Has Lasted Long Enough to Be Considered Chronic
Chronic pain is typically defined as pain that persists beyond normal healing timelines. If your pain has continued for 3–6 months or longer, it may be time to consider more advanced solutions.
Common indicators include:
- Pain that interferes with sleep or keeps you from getting restorative rest
- Reduced ability to walk, stand, or sit comfortably
- Difficulty working, commuting, or concentrating
- Missing out on hobbies, social activities, or time with family because pain dictates your choices
Conservative Treatments Haven’t Delivered Durable Relief
Many people consider SCS after they’ve genuinely tried standard options, such as:
- Physical therapy and guided rehabilitation
- Medications
- Targeted injections
- Lifestyle changes (movement modification, sleep strategies, weight management, stress reduction)
You Want to Reduce Medication Dependence
A major reason people seek SCS is the desire to step away from constant medication as the primary strategy.
You may relate if you have:
- Concerns about long-term side effects, tolerance, or diminishing benefit
- A desire for more consistent symptom control rather than “peaks and crashes”
- A goal of feeling more stable and functional without relying on sedating or high-risk medications
Your Symptoms Match Nerve-Related Pain
Spinal cord stimulation is typically most effective for neuropathic pain (nerve-driven pain). Symptoms often include:
- Tingling or “pins and needles”
- Numbness
- Burning sensations
- Hypersensitivity (pain from light touch or normal pressure)
- Pain that radiates or “travels,” such as down the leg or into the foot, rather than staying in one spot
The Truth About the SCS Trial: “Try Before You Commit”
One of the most reassuring parts of spinal cord stimulation is that it typically involves a trial period before any permanent implant is considered. This “try before you commit” approach matters because it reduces guesswork and helps patients make decisions based on real-life results.
What to Expect During the Trial
Most SCS trials involve:
- Temporary leads
- Thin wires placed to deliver stimulation to targeted nerve pathways
- These are not permanent and are used only for the trial period
- A short trial period to test symptom improvement
- The goal is to see whether stimulation reduces pain enough to improve daily life
- Many patients use this time to test common triggers (walking, sitting, sleeping, errands)
- Daily activity evaluation
- You’ll pay attention to what changes: pain levels, sleep, walking tolerance, ability to do normal routines
- This real-world testing is what makes the trial so valuable
What “Success” Looks Like
Success doesn’t have to mean “zero pain.” A realistic definition is:
- Meaningful improvement in pain intensity and/or function
- Better sleep, more stable days, fewer flare-ups
- Being able to do more of what matters with less suffering
Benefits Buckhead Patients Often Look For With SCS
Potential Improvements
Patients often hope to achieve:
- Reduced pain intensity, especially nerve pain
- Better sleep and more consistent daily function
- Improved walking or standing tolerance
- Less reliance on pain medications (when appropriate and clinically safe)
Quality-of-Life Outcomes That Matter
For many people, the real wins look like:
- Returning to hobbies and activities they had to give up
- Being more present with family—without pain dominating every moment
- Feeling hopeful again because progress finally feels possible
The “Control” Element
Many SCS systems allow a degree of personalized control (as appropriate), meaning:
- Settings may be adjusted to match daily needs—like activity, rest, or sleep
- The experience can be optimized over time with follow-up and fine-tuning
Get Clarity Without Pressure
Chronic pain is real—and it deserves more than rushed appointments, vague answers, or “just live with it” advice. If you’ve been dealing with persistent nerve pain, the most important next step is finding a care team that takes a thoughtful, least-invasive approach, grounded in accurate diagnosis and honest guidance.
If you’re living with chronic nerve pain and wondering whether spinal cord stimulation could help, the team at Medici Orthopaedics & Spine is here for you. We take time to understand your history, identify the true source of pain, and walk you through your options—including minimally invasive treatments and spinal cord stimulation—so you can make a confident decision.
Contact Medici Orthopaedics & Spine
📞 Main Appointment Line: 1-844-328-4624
🌐 Website: https://www.mediciortho.com
Clinics
- Kennesaw:
2911 George Busbee Parkway, Suite 50, Kennesaw, GA 30144
(770) 545-6404 - Snellville:
2220 Wisteria Drive, Unit 101, Snellville, GA 30078
(470) 645-9297 - Buckhead PM&R:
3200 Downwood Circle NW, Suite 520, Atlanta, GA 30327
(770) 872-7549









